Customer Story
From Billing Chaos to Control: A Medicaid Recovery Story
- $30,000+ in backlogged claims recovered – including denials tied to the Pathways billing shift
- 100% confidence in billing – with expert training, real-time support, and system guidance
- Clear Medicaid navigation – even through evolving state rules and Pathways requirements
- Peace of mind during growth – more time to scale, less time chasing payments


Experts at Medicaid Billing:
Getting you 98% claims approved upon first claim submission.
Powerful Software that Drives Your Medicaid Agency
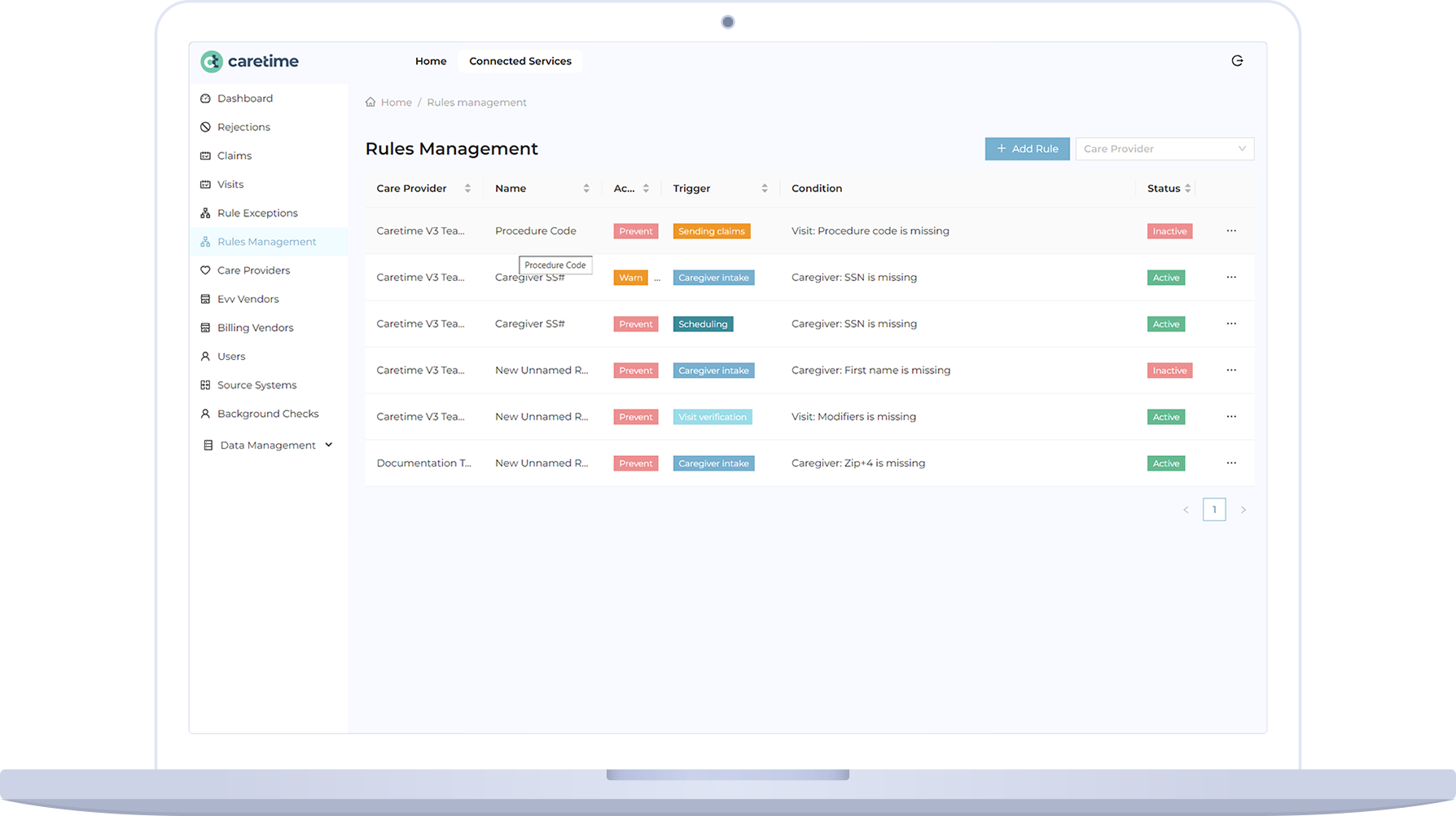
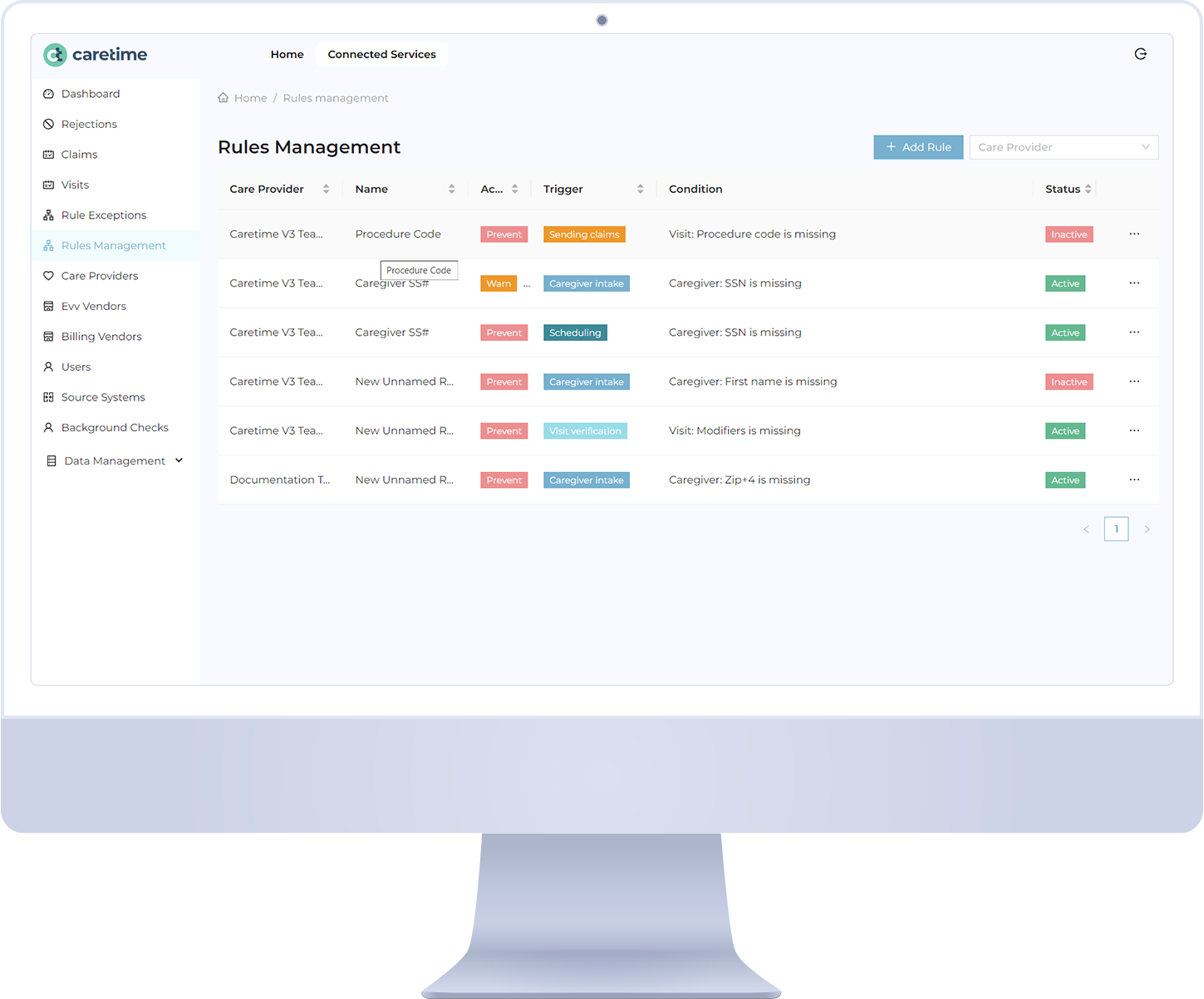
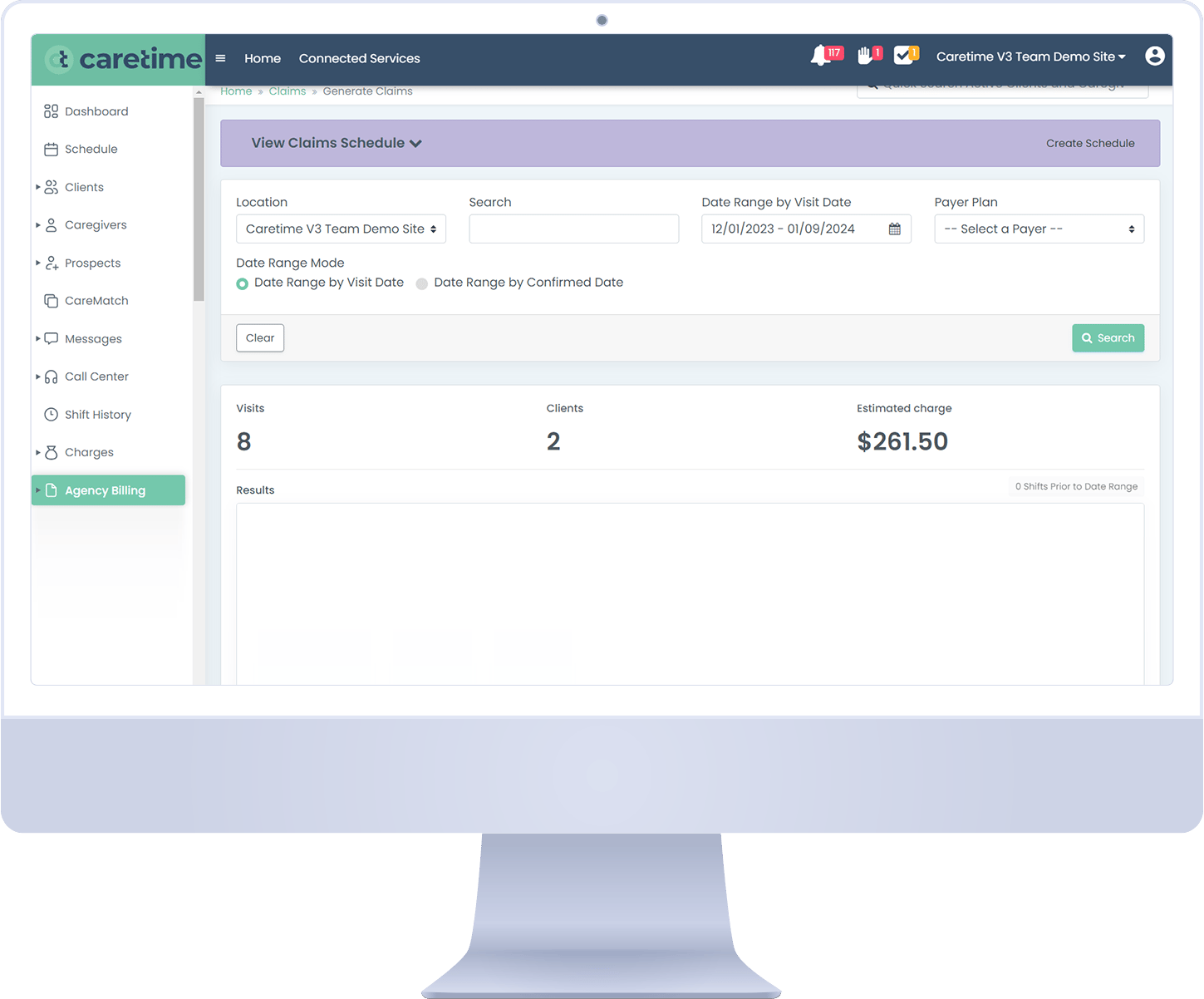
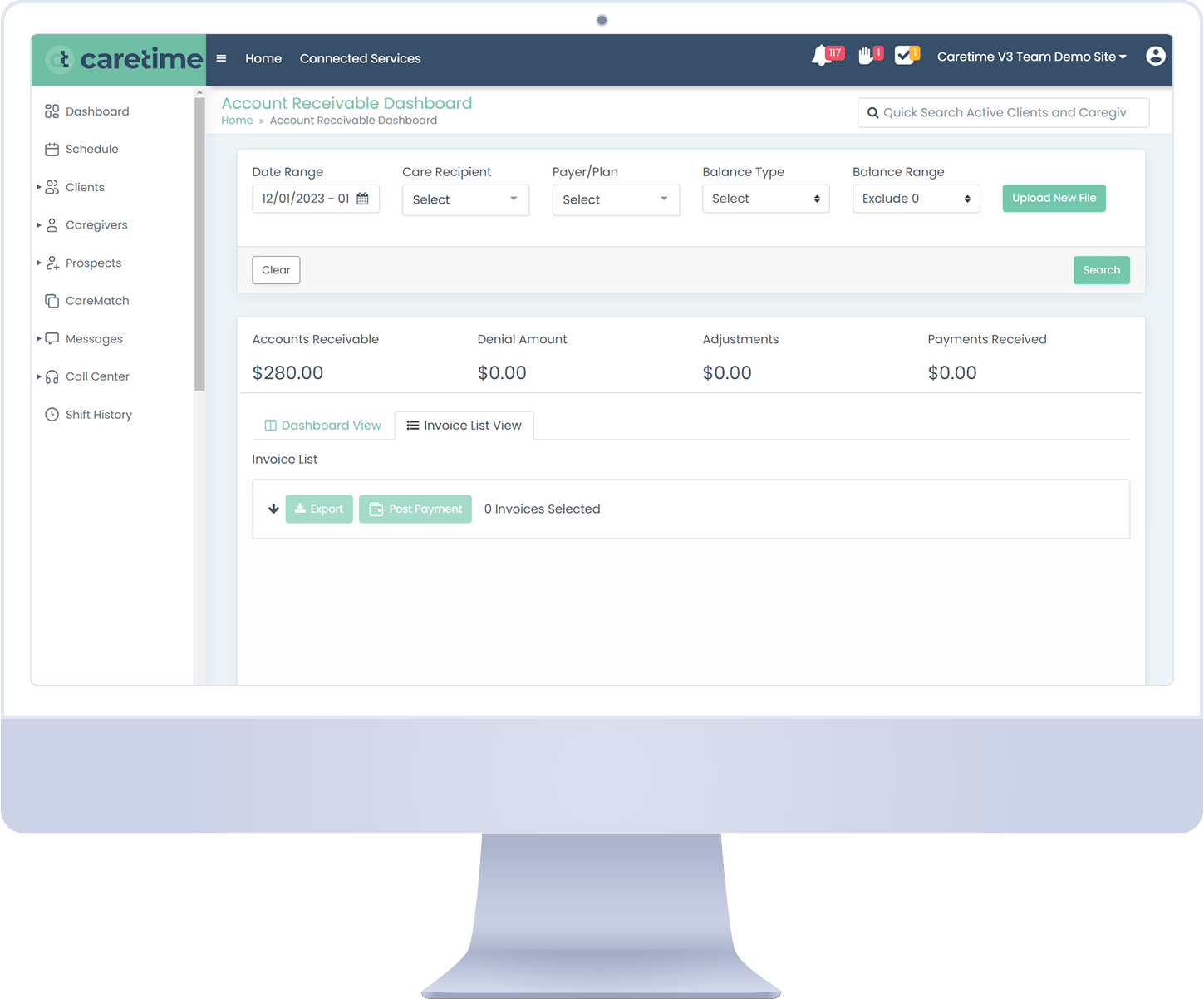
Accurate Claims Management
What does this mean for you? We ensure precision in claims submission with automated checks and balances that reduce errors and denials AND improve your reimbursement rates and financial performance.
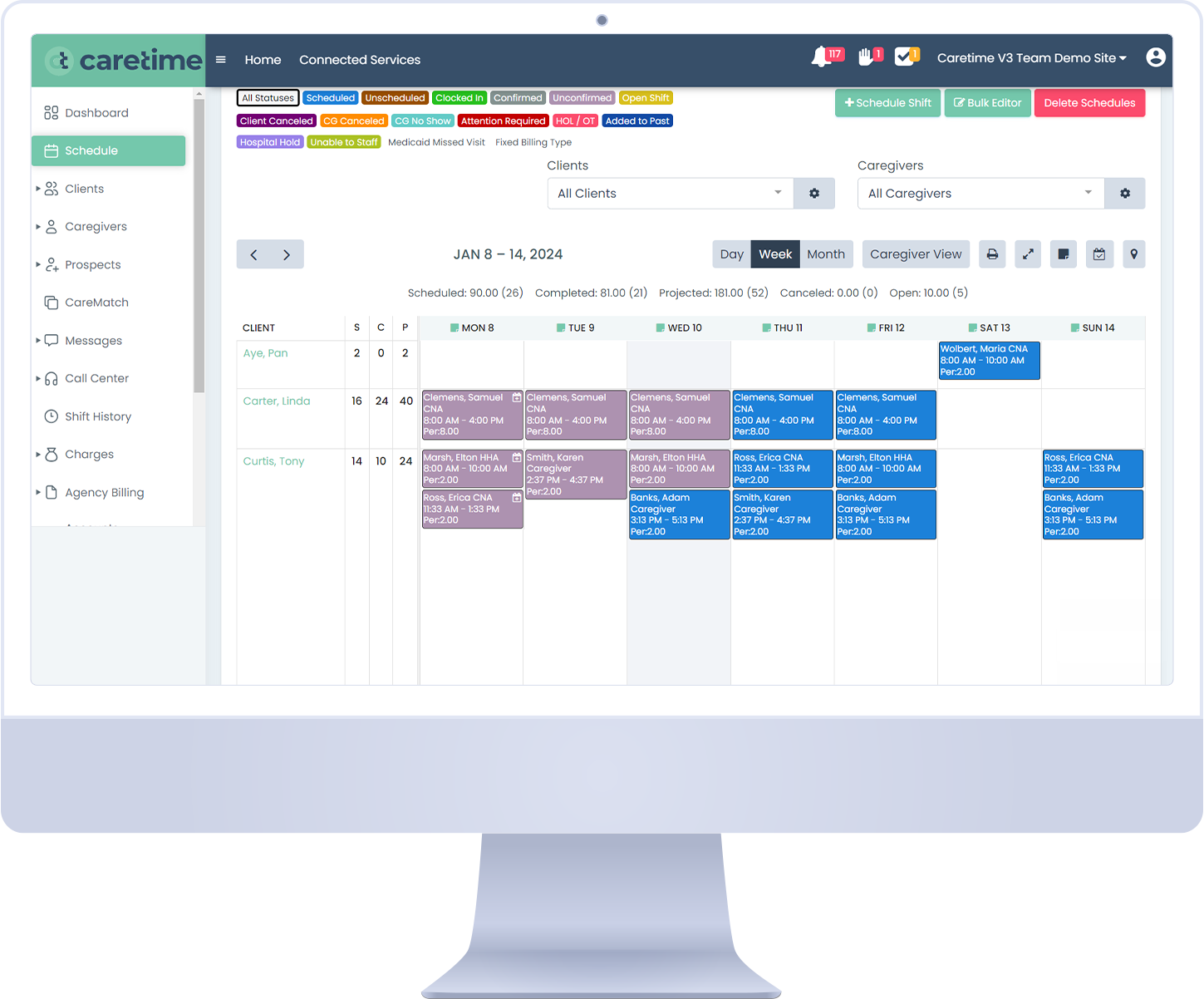
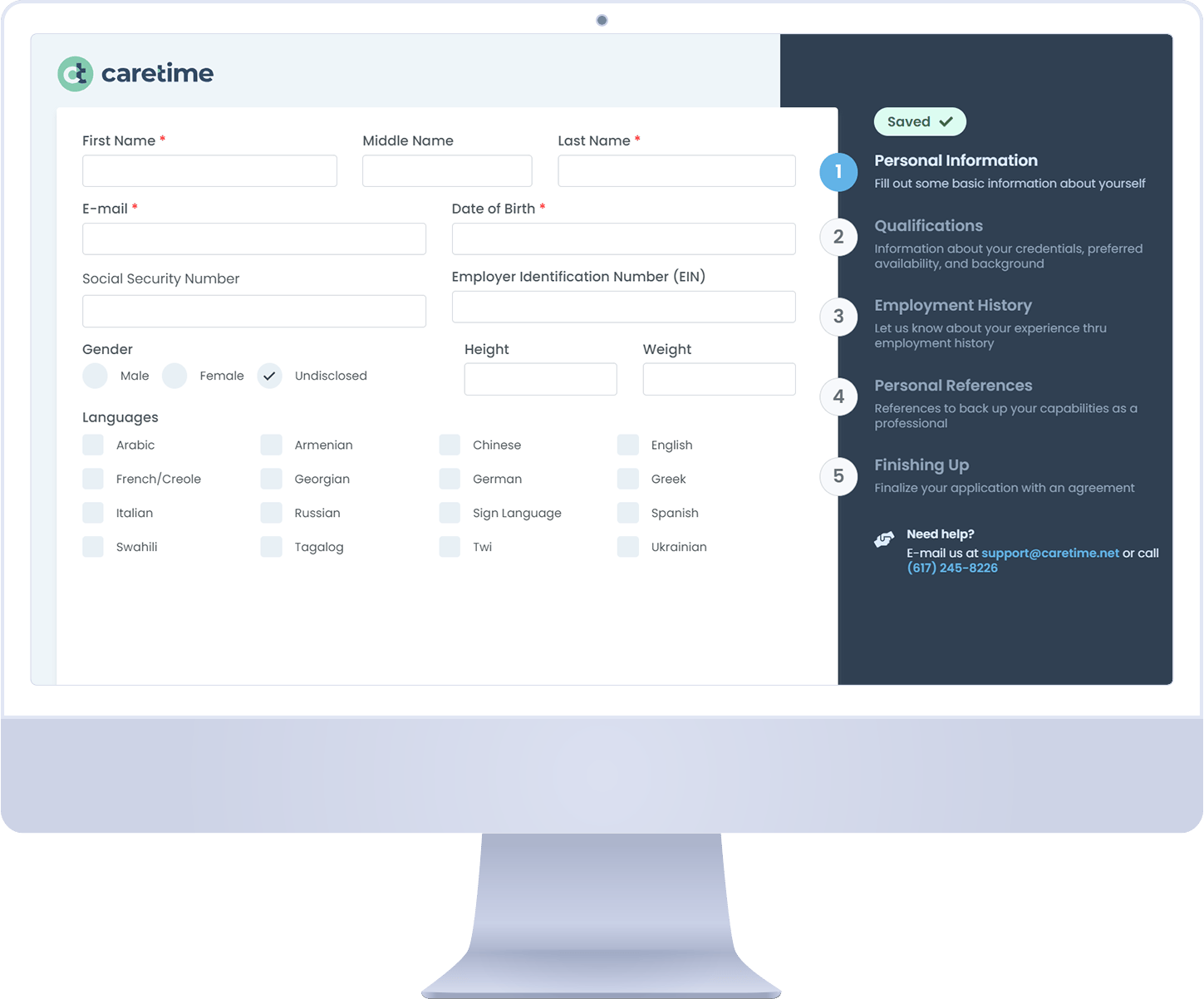
Reliable EVV
Integrated seamless EVV capabilities that ensure accurate and verifiable records of service delivery that are compliant and enhance agency accountability and operational transparency.
Comprehensive Compliance
Stay ahead of regulatory changes with updated real-time tools ensuring that your billing practices meet state and federal Medicaid requirements.
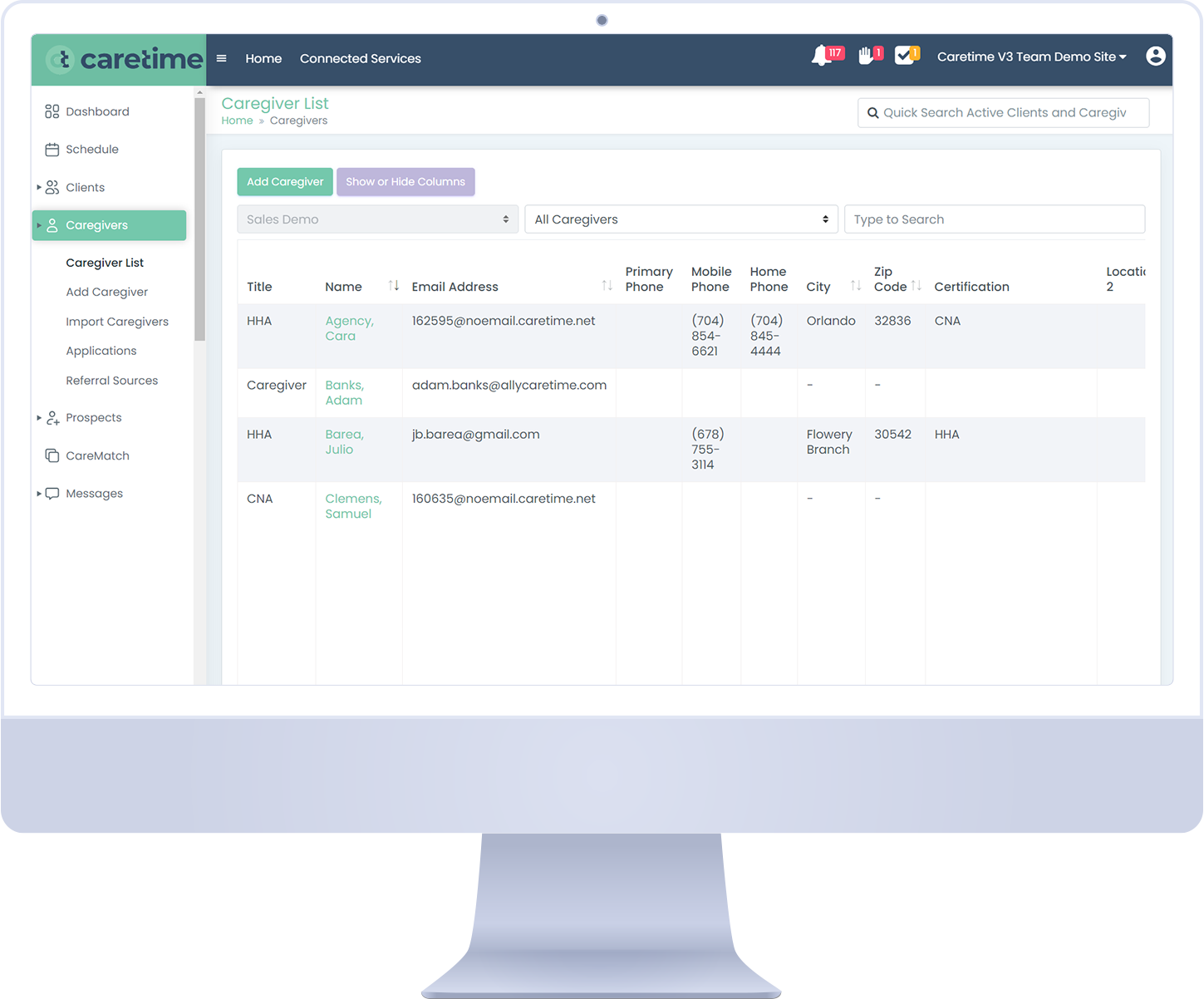
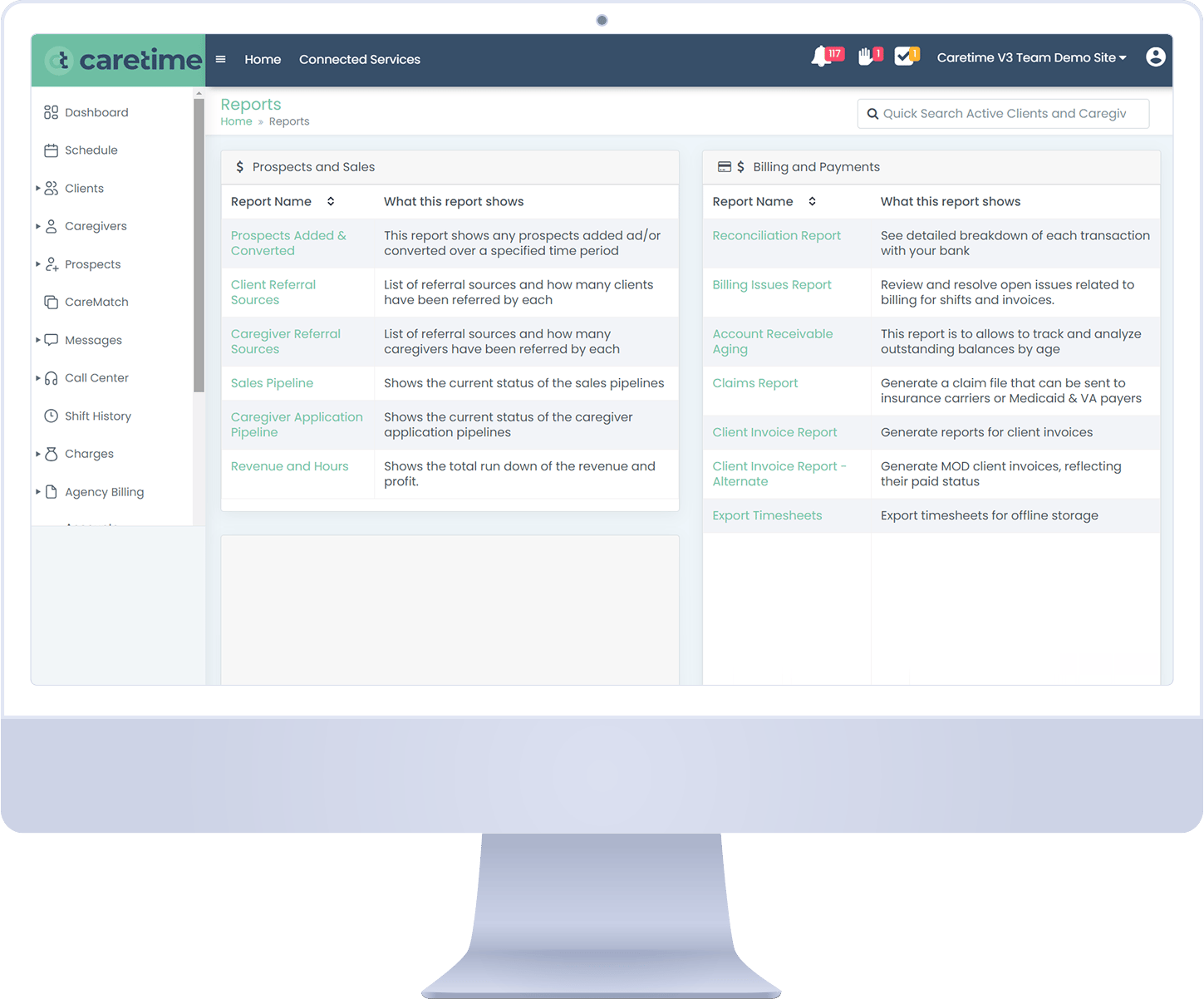
Better Insights
Advanced analytical and reporting tools that provide reliable and useful information that can be used to improve performance, processes and client outcomes.
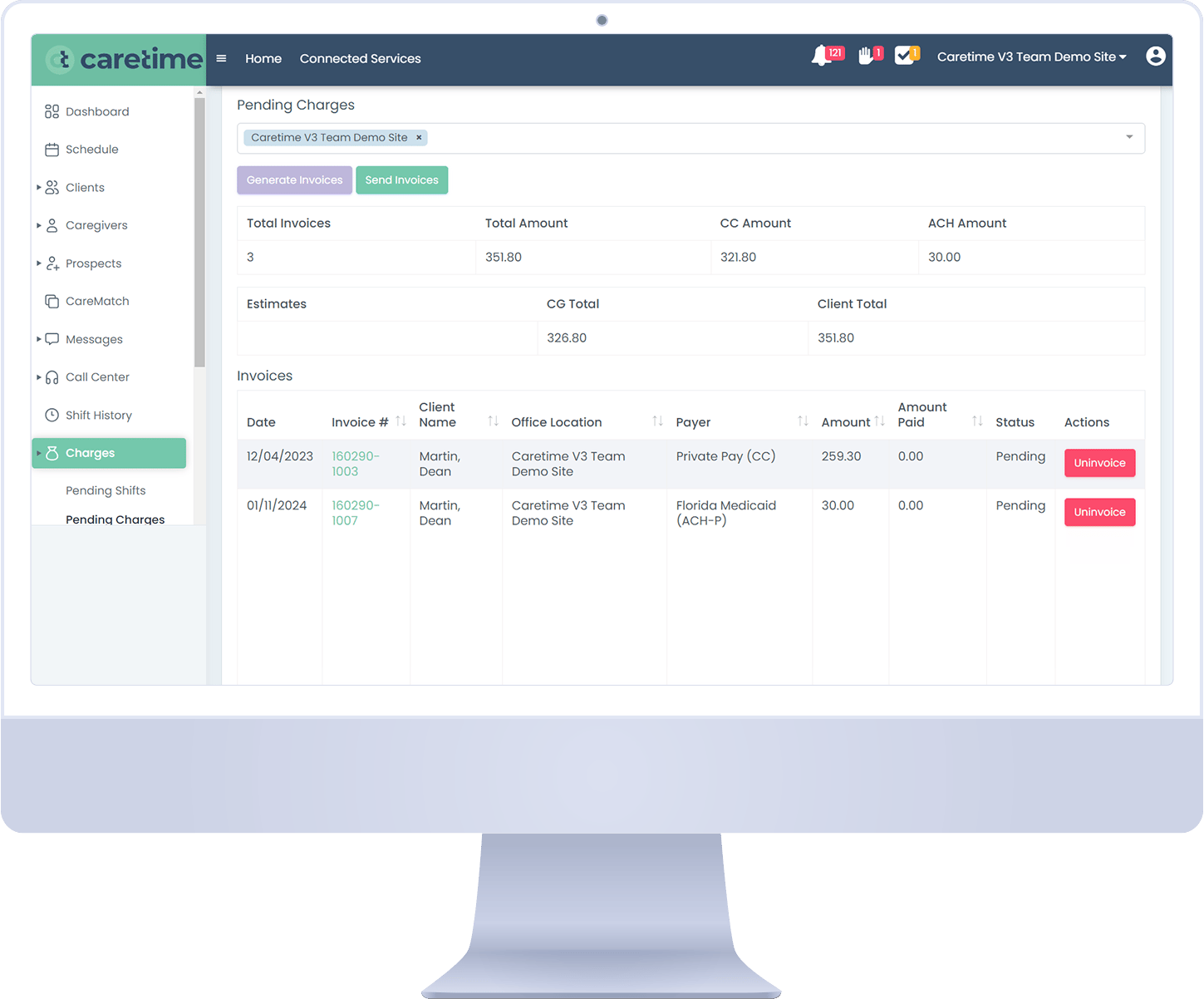
Enhanced Billing Efficiency
Designed to minimize administrative overhead and reduce time from delivery to payment.
Clearinghouse Choices
Choose your preferred clearinghouse rather than being locked in to a single provider.

Curious, even just a bit? Schedule a meeting, it's worth a conversation.
Are you currently a CareTime user looking for support? Click here.


%20(1920%20x%201080%20px)%20(1).jpg)